Tissue Thickness overlying ischial tuberosity in a simulated sitting posture measured on MRI images
Mohsen Makhsous, PhD1-4 , Andrew Cichowski1-2 , Iris Cheng1-2 , Andy Lee2 , Mauli Modi, MS1-2 , Fateme Esfanduarpour2 , Thomas Grant, DO5 , Fang Lin, DSc1-3
Departments of 1 SMPP, Rehabilitation Institute of Chicago, 2 PTHMS, 3 PM&R, 4Orthopaedic Surgery, 5 Radiology, Northwestern University, Chicago, Illinois, USA 60611
ABSTRACT:
To investigate the changes of the tissue thickness overlying the ischial tuberosity (IT) from the Supine to Sitting posture, as well as the changes between Non-Weight-Bearing and Weight-Bearing in sitting, eleven healthy subjects were tested in supine and simulated sitting postures in MRI for 4 conditions (Supine, 45° Hip Flexion, Non-Weight-Bearing Sitting and Weight-Bearing Sitting). The thickness of the tissue layers was measured between the tip of IT and the skin from the images. The gross soft tissue overlying IT was found to be significantly thinner in sitting than that in supine. The decrease of tissue thickness was not uniform among the layers. The muscle thickness decreased substantially more than the others. Muscle thickness further decreased from Non-Weight-bearing Sitting to Weight-bearing Sitting by 46.2±7.9%. Findings confirmed that there are significantly less padding tissues around IT in a seated posture and sitting load applied through IT significantly compressed the muscle tissue.
Key words:
seated posture; buttock; gluteus maximus; magnetic resonance imaging; ischial tuberosity, in vivo.
INTRODUCTION:
Pressure ulcer development can initiate in deep muscle closer to bony prominence due to excessive deformation3. It is reported that the buttock anatomical structure in a sitting posture may be different intuitively from that in a supine or standing posture2. However, there is a lack of evidence in the literature regarding such a difference in terms of tissue thickness overlying the ischial tuberosities. In particular, coverage of the ischial tuberosity (IT) by the gluteus maximus muscle may vary as the hip joint flexes because muscles may change shape and may interact with each other and with underlying bones. Thus, the IT may have less padding tissue to resist the pressure load during sitting. Therefore, the tissue structure overlying the IT needs to be studied in a sitting posture to increase our knowledge about the structural changes in sitting. The objective of this study was to measure the soft-tissue thickness around the IT through MRI images obtained in a seated posture. We hypothesized that the region immediately beneath the ischial tuberosities in a sitting posture has less soft-tissue thickness than that in a standing/supine posture and thus the IT will be significantly less covered by the soft tissue with the flexion of the hip joint. It was also hypothesized that under a weight-bearing upright sitting posture the soft-tissue thickness will be less due to the deformation of the tissue under the body weight.
METHODS:
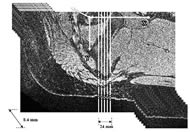
Eleven healthy subjects (age 35.9±6.5 years, height 162.9±6.5 cm, weight 56.7±6.0 kg, BMI 21.4±2.3 kg/cm2; 6 female and 6 male) participated in the MRI study. The inclusion criterion was height less than 170 cm, in order to fit into the tight space in MRI to simulate a sitting posture (Fig. 1). The exclusion criteria were the general rules for MRI recording. Informed and written consent following the guidelines of the Institutional Review Board was obtained from each subject before any experimentation.
Postures and loading conditions:
Subjects were positioned in a 1.5T MRI scanner (Magnetom Espree, Siemens Medical Systems Inc., Malvern, PA) in the following postures and loading conditions: Supine: Subject was laying in a supine posture with both the hip and knee joints fully extended. 45º Hip Flexion: Subject was laying in a supine posture with the hip 45º flexed and the knee 90º flexed. Non-Weight-Bearing Sitting: Subject was laying in a posture with the hip and the knee close to 90º flexed without any load in the buttock regions. Weight-Bearing Sitting: Subject was laying in an upright posture with the hip and the knee close to 90º flexed while the buttock regions were loaded.
To mimic a sitting posture in a MRI tube, an apparatus was constructed using foam blocks (Fig. 1) to keep hip and knee at close to 90º flexion (Fig. 1). To apply a pressure load to the posterior side of the buttocks and thighs, the cushion under the subject’s buttock-thigh was designed as a sandwich structure, consisting of two layers of stiff materials with rectangular air bladders in between. The air bladders were inflated and deflated through the connection of long plastic tubing to an air pump outside of the MRI room. The simulated sitting load was comparable to the subject’s actual sitting load measured in an upright sitting posture in a regular office chair, prior to the MRI recording.
Protocol and data processing:
Subjects were positioned in the MRI scanner and volumetric MR images of the right buttock-thigh (576x576 matrix, 35cm FOV, 288 slices, 0.6mm thickness) were obtained in the above 4 conditions. The thickness of the tissue layers between the IT and the skin was measured from the MRI images using a custom MATLAB (Matlab R2008a, The MathWorks, Inc., Natick, MA) code. For each condition, 15 consecutive sagittal images were first selected manually with the one at the tip of the IT as the center slice. For each image, 5 vertical lines were automatically aligned parallel to the superior-inferior axis, 6mm apart, with the center line passing through the referenced IT tip. The measurement of the tissue thickness was performed by picking 4 points along each of the vertical lines where the lines encountered the boundaries of each layer, i.e. bone, muscle, fat and skin (Fig. 2).
Statistical Analysis:
An ANOVA with repeated measures was used to detect any significant effect of hip angle on tissue thickness and any significant difference among the 3 tissue layers of skin+subcutaneous, fat, and muscle. For effect of the loading (Non-Weight-Bearing Sitting and Weight-Bearing Sitting) on the soft-tissue thickness, a t-test was used to detect any difference for each layer (skin, fat, and muscle). All statistical tests were done using SPSS 16.0 (SPSS Inc., Chicago, IL) with the significance level of 0.05.
RESULTS:
Gross soft-tissue thickness:
Gross soft-tissue experienced significant (P< 0.001) decreases in thickness from Supine to 45° Hip Flexion, and from Supine to Non-Weight-bearing Sitting. In addition, gross soft-tissue thickness was significantly decreased (P<0.001) in Weight-Bearing Sitting as compared to the Non-Weight-Bearing Sitting.
Muscle thickness:
Muscle thickness was significantly (P<0.001) larger than the fat thickness in Supine posture but not in either 45° Hip Flexion or Non-Weight-bearing Sitting (Fig. 3A). The effect of the hip flexion angle was significant (P<0.001) on the muscle thickness. Muscle tissue experienced significant (P< 0.001) decreases in thickness from Supine posture to 45° Hip Flexion, and from Supine to Non-Weight-bearing Sitting. Moreover, muscle tissue experienced a significant (P< 0.001) decrease in thickness from Non-Weight-bearing Sitting to Weight-bearing Sitting (Fig. 3B).
Fat tissue experienced a significant decrease in thickness from Non-Weight-bearing Sitting to Weight-bearing Sitting (P=0.001). Skin and subcutaneous tissue thickness was significantly (P<0.001) smaller than the fat and muscle thicknesses in all postures (Fig. 3A).
DISCUSSION:
This study has confirmed that the soft-tissue thickness around the IT in a sitting posture is different from that in a standing or supine posture. The soft tissue overlying the IT was found to be significantly thinner in a seated posture than it is in a supine posture even when there is no sitting load. This finding says that hip flexion alone can bring forth a significant decrease in soft tissue thickness underneath IT. In addition, we found that the decrease of tissue thickness is not uniform among the tissue layers in area around IT. The decrease of thickness in muscle tissue was substantially more than that in fat and skin tissues. Therefore, when sitting pressure is applied to tissue layers with decreased thickness, the muscle tissue may be more susceptible to pressure injury than fat or skin tissues.
The pressure of a sitting load compressed the soft tissues to decrease in thickness by nearly one half of its initial unloaded thickness in the same sitting posture.
The results from our data under Weight-Bearing Sitting favorably correspond to the fact that serious skin breakdown in the spinal cord injury (SCI) population has been reported frequently over the ischial tuberosities1 , which may be due to less padding tissue to resist the concentrated high pressure over bony prominences. Unfortunately, it was found that the gluteus muscle thickness under the ischial tuberosities in individual with chronic SCI is decreased close to half the thickness of these muscles in healthy individuals 4 . Thus, the thin muscles overlying the ischial tuberosities of individuals with SCI bear highly elevated mechanical stresses due to less padding tissue under sitting with sustained bodyweight loading.
REFERENCES
- Ankrom, M. A.; Bennett, R. G.; Sprigle, S.; Langemo, D.; Black, J. M.; Berlowitz, D. R.; and Lyder, C. H.: "National Pressure Ulcer Advisory Panel. Pressure-related deep tissue injury under intact skin and the current pressure ulcer staging systems". Adv Skin Wound Care 18: 35-42, 2005.
- Kaplan, R. L.: Physical Medicine & Rehabilitation Pearls of Wisdom. 1 ed. Lincoln: Boston Medical Publishing Corporation, 225. Edited, 2003.
- Kosiak, M.: Etiology and pathology of ischemic ulcers. Arch Phys Med Rehab, 40: 62-9, 1959.
- Linder-Ganza, E.; Shabshinb, N.; Itzchakb, Y.; Yizhar, Z.; Siev-Ner, I.; and Gefen, A.: Strains and stresses in sub-dermal tissues of the buttocks are greater in paraplegics than in healthy during sitting. Journal of Biomechanics, 41(3): 567-80, 2008.
ACKNOWLEDGEMENT:
The project was supported by NIH Award #K25 HD051983-01A1.
Correspondence Author:
Mohsen Makhsous, Dept of Physical Therapy & Human Movement Sciences, Northwestern Univ., 645 N. Michigan Ave., Suite 1100, Chicago, IL 60611. Phone 312-503-0073. Email: m-makhsous2@northwestern.edu